The Hidden Signs of Insulin Resistance and How to Reverse It Naturally
If you’re constantly craving sugar, struggling to shift stubborn weight or feel like your energy crashes before the day is done, insulin resistance could be quietly working behind the scenes. This condition often flies under the radar, affecting people for years before it gets picked up. The frustrating part? Many of the early signs are dismissed as just being busy, getting older or not sleeping well enough.
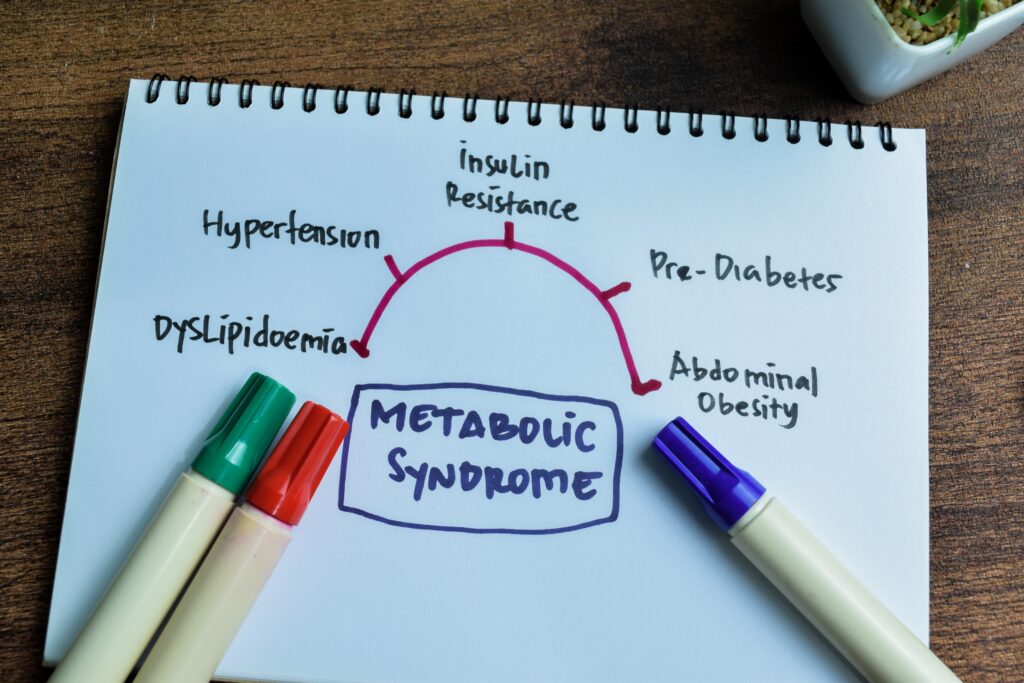
Insulin resistance happens when your cells stop responding properly to insulin, the hormone that helps move glucose from your bloodstream into your cells for energy. When your body becomes less sensitive to insulin, blood sugar and insulin levels stay high. Over time, this can lead to weight gain, fatigue and, eventually, type 2 diabetes. According to one study, insulin resistance is a leading driver of metabolic syndrome, which affects up to one in four adults globally. It’s more common than you might think, especially in women over 40, those with PCOS or anyone juggling chronic stress, poor diet and a lack of movement.

Why insulin resistance is often missed
The thing about insulin resistance is that it’s quiet. It builds slowly, without dramatic symptoms at first. Many people don’t know they have it until they start gaining weight without explanation or their blood sugar starts creeping into the pre-diabetic range. Because fasting glucose tests can still appear normal in the early stages, insulin resistance often goes undetected.
Who is at risk?
Hormonal changes during perimenopause and menopause make women particularly vulnerable. Oestrogen helps maintain insulin sensitivity, so as levels drop, the body naturally becomes more resistant to insulin. In younger women, PCOS often comes with insulin resistance as a core feature. High stress, sleep deprivation and sedentary habits also increase the risk, creating a perfect storm.

The hidden symptoms of insulin resistance
People often associate insulin resistance with weight gain, but its effects are more wide-reaching than most realise. One of the most common red flags is unexplained weight gain around the middle, even if your eating habits haven’t changed. This visceral fat is more metabolically active and strongly linked to insulin resistance.
Sugar cravings can feel relentless as the body becomes dependent on a quick glucose hit to stay energised. Fatigue is another big clue, especially when paired with brain fog or that 3pm slump that just won’t budge. You might find yourself constantly hungry, even after meals, and always looking for something to snack on.
Physical signs include darkened patches of skin known as acanthosis nigricans, especially around the neck or armpits. Skin tags are also common. On the hormonal side, irregular cycles, worsening PMS or perimenopausal symptoms can suggest insulin is off.
Sleep disturbances and waking up unrefreshed are classical symptoms too. One study found that people with insulin resistance were more likely to report poor sleep quality. High blood pressure, abnormal cholesterol levels, increased thirst and frequent urination also point to blood sugar problems.
How to test for insulin resistance
Fasting glucose tests alone don’t always catch insulin resistance early. For a more accurate picture, several other lab markers are worth exploring. Fasting insulin levels are one of the best places to start. Most experts consider anything below 5 mIU/L to be optimal, even though many labs list the upper limit at 25.
The HOMA-IR score, which combines fasting glucose and insulin, gives a clearer snapshot of insulin sensitivity. A score under 1.0 is generally ideal. HbA1c reflects average blood sugar over the past three months, with anything above 5.7 per cent edging into prediabetic territory. Finally, the triglyceride-to-HDL ratio is a well-established marker of metabolic health. A ratio below 1.5 is a good target, according to published data.
How to reverse insulin resistance naturally
The best news? Insulin resistance is highly responsive to lifestyle changes. You don’t need extreme diets or fancy supplements to make progress. What your body really needs is consistency and nourishment.

Diet and nutrition
Start by focusing on protein. Including it in every meal helps slow digestion and keep blood sugar steady. Fibre-rich foods like leafy greens, beans and oats not only improve gut health, but also increase insulin sensitivity. Healthy fats from avocado, olive oil and nuts support hormonal balance and help you feel satisfied.
Cutting back on refined carbs and added sugars is essential. These foods cause sharp blood sugar spikes, followed by crashes that leave you hungry and tired. Eating three balanced meals a day, rather than grazing constantly, gives your body a chance to reset.
Some women benefit from intermittent fasting, particularly a 12:12 or 14:10 window. But fasting doesn’t suit everyone. If it causes anxiety, fatigue or worsens hormonal symptoms, it may not be the right fit.
Exercise for insulin sensitivity
Exercise is a game-changer. Strength training is particularly effective because it builds muscle, and muscle is the most insulin-sensitive tissue in the body. Walking after meals is simple but powerful—it helps muscles absorb glucose more efficiently. Even just ten minutes can lower blood sugar. High-intensity interval training (HIIT), done in moderation, can further improve glucose metabolism, according to findings.
Lifestyle and stress management
Stress is often the elephant in the room. Chronic stress keeps cortisol high, and high cortisol worsens insulin resistance. Meditation, slow breathing, time in nature or journalling can all help lower cortisol and support hormonal balance. Prioritising sleep is just as important. Research shows that sleep deprivation reduces insulin sensitivity by up to 30 per cent after just one night.
Gut health matters too. A diverse microbiome helps regulate blood sugar and reduce inflammation. Fermented foods like sauerkraut and kefir, along with prebiotics found in garlic, onions and asparagus, can support this. Magnesium is another overlooked nutrient. Studies show that supplementing with magnesium improves insulin sensitivity, especially in people with low levels.
The bottom line
Key takeaways and next steps
Insulin resistance is more common than many realise, and it can affect your energy, weight and hormones long before blood sugar tests raise red flags. But the earlier you catch it, the easier it is to turn things around. If you’re feeling off and the usual strategies aren’t working, testing your insulin and related markers can be an empowering first step.
Small changes add up. Prioritising protein and fibre, building muscle through strength training, managing stress and sleeping well are some of the most effective ways to restore insulin sensitivity. You don’t need to be perfect—you just need to support your body in the way it needs most right now. With the right approach, you can rebalance your blood sugar, boost your energy and protect your long-term health.





